Fecal Transplants, Postbiotics, and Rebuilding Gut Health for the Most Sensitive Patients
Jun 26, 2025
When it comes to healing the gut, some of the most challenging cases require more than just a probiotic or food elimination diet. We’re talking about individuals with deeply imbalanced microbiomes: those who live with chronic bloating, frequent illness, post-antibiotic fallout, or autoimmune symptoms that haven’t responded to conventional care.
These are the people who’ve “tried everything” and still don’t feel like themselves.
For sensitive systems like these, gut health restoration requires advanced tools. While fecal microbiota transplants (FMT) have made headlines for their ability to reset the microbiome, there's now an even more accessible, targeted, and less invasive solution: postbiotic therapy using ThaenaBiotic.
This blog explores what fecal transplants are, why they’re mostly off-limits in the U.S., and how postbiotics are stepping in as the future of healing the microbiome naturally.
Especially when conventional options fall short.
What Is a Fecal Microbiota Transplant (FMT)?
A fecal microbiota transplant (FMT) is a medical procedure that transfers stool from a healthy donor into the colon of a patient. The goal is to restore microbial balance in the gut. The transplant essentially repopulates it with beneficial bacteria and microorganisms that may be missing due to illness, antibiotic use, or chronic inflammation.
Donor stool is rich in a diverse range of microbes that play essential roles in digestion, nutrient absorption, immune modulation, and inflammation control. With the introduction of new microbiota into a compromised gut, FMT helps reestablish diversity and function in the gut ecosystem.
For people struggling with conditions like recurrent infections or those who’ve experienced microbiome collapse post-antibiotics, FMT has been a beacon of hope and one of the few proven tools for gut health restoration.
Why Is FMT Used?
FMT is most commonly used to treat a very specific and severe condition: recurrent Clostridium difficile (C. diff) infections. C. diff is a dangerous bacterial infection that causes severe diarrhea, abdominal pain, and potentially life-threatening complications. It often arises after antibiotic use, which can wipe out the good bacteria that usually keep C. diff in check.
According to a landmark study published in The New England Journal of Medicine, fecal transplants have an 85–95% success rate in resolving recurrent C. diff infections. This makes it one of the most effective treatments available for patients who have not responded to traditional antibiotics or those seeking a stool transplant for C. diff.
FMT restores a microbial diverse environment that naturally suppresses the overgrowth of harmful bacteria and supports a healthier, more functional digestive system.
How Is a Fecal Transplant Done?
There are several methods for administering an FMT, depending on the patient’s condition and preferences:
- Colonoscopy: This is the most direct method, delivering the donor material deep into the colon.
- Enema: Less invasive, but often less thorough.
- Upper endoscopy: Introduces the stool through the stomach or small intestine.
- Capsules: Freeze-dried donor stool in capsule form, designed to release in the digestive tract.
Each method has its own pros and cons, and all require rigorous donor screening, lab processing, and sterile conditions to ensure safety. Because of the complexities involved, FMT is usually reserved for serious clinical cases under strict supervision.
And while the concept of a “stool transplant” might sound extreme, for some, it’s the only thing that has brought real relief.
Still, there’s a catch.
Why Fecal Transplants Are Largely Unavailable in the U.S.
Although fecal transplants sound like a promising solution for many gut-related conditions, they are heavily regulated in the United States. The FDA currently limits FMT to treating only patients with recurrent C. diff infections who have failed conventional treatment. This means:
- FMT is not legally approved for IBS, IBD, autoimmune disease, food sensitivities, or “general gut health,” leaving those in search of a fecal transplant alternative.
- There are no FDA-approved fecal transplant alternatives for broader use cases.
- Clinics offering off-label FMT are likely operating in a legal gray area or potentially outside the law entirely.
So, what happens when someone’s microbiome is severely out of balance, but they don’t qualify for a stool transplant? Are they just out of options?
Fortunately, options like postbiotic therapy for sensitive guts are gaining traction as more providers shift to healing the microbiome naturally.
What Are Postbiotics?
You’ve probably heard of prebiotics and probiotics. But postbiotics are where the magic really happens.
Think of postbiotics as the language your microbiome uses to talk to your body. They regulate inflammation, support digestion, and restore gut-brain communication. All without the risks that sometimes come with live bacteria.
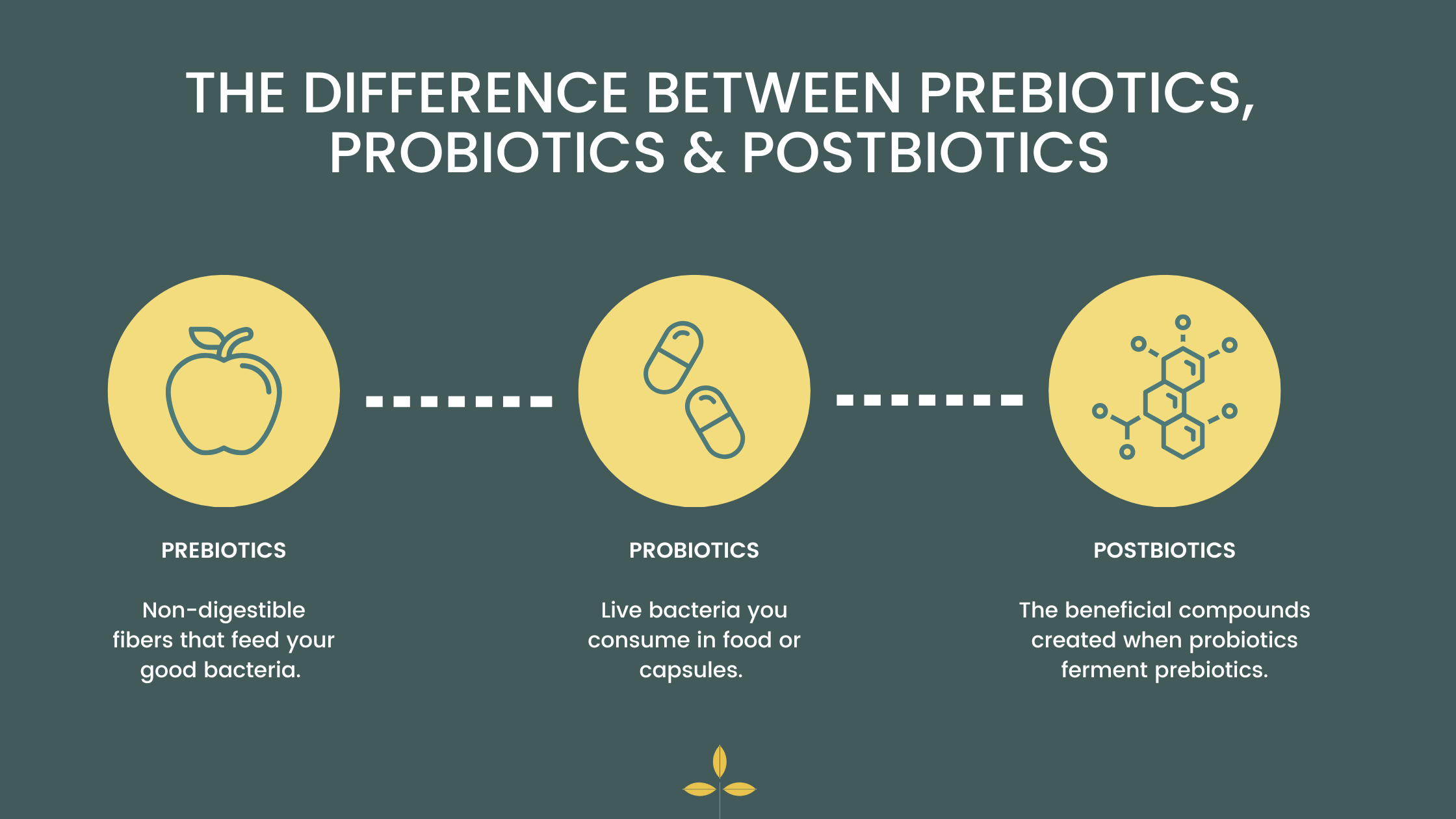
Postbiotics include:
- Short-chain fatty acids (like butyrate)
- Enzymes
- Peptides
- Communication molecules that interact with your immune system and gut lining
Many practitioners are shifting to postbiotic-first protocols for the most sensitive cases.
Postbiotic Therapy with ThaenaBiotic
ThaenaBiotic is a clinically developed, stool-derived postbiotic supplement. It mimics many of the benefits of a fecal transplant but in a safer, more targeted, and much more accessible form. It’s designed for people who are intolerant to probiotics or need microbiome support post-antibiotics.
Unlike probiotics, which introduce live bacteria into the gut (with mixed results), postbiotics deliver the compounds those bacteria create. These are the bioactive byproducts that interact directly with your cells in various parts of your body to support immunity and repair.
Here’s what makes ThaenaBiotic so unique in the world of microbiome support:
- It’s derived from screened, healthy donor stool but the bacteria are completely inactivated, so it’s safe and sterilized. What remains are postbiotics, peptides, and prebiotic fibers, with no risk of infection.
- No live organisms which benefit clients with SIBO or histamine issues who can’t tolerate traditional probiotics.
- It’s only available through trained providers, ensuring it’s used appropriately and effectively.
- This postbiotic supplement is specifically formulated for people with fragile microbiomes and ongoing inflammatory or immune responses.
For those seeking microbiome support post-antibiotics, or a safer way to rebuild gut health after illness, ThaenaBiotic is a research-backed, professional-grade solution.
Who Can Benefit from Postbiotic Therapy?
ThaenaBiotic and postbiotic therapy can be life-changing for people with:
- Chronic bloating or IBS/IBD
- Autoimmune diseases like Hashimoto’s or lupus
- Food sensitivities and histamine intolerance
- Post-antibiotic gut issues
- Post-COVID digestive symptoms
- Children and adults who don’t tolerate probiotics
- Those seeking an effective fecal transplant alternative
If you’ve tried probiotics, elimination diets, or even antibiotics without lasting relief, postbiotic therapy for a sensitive gut might be the missing piece.
Why You Need a Qualified Provider to Guide You
Healing a damaged microbiome takes more than just supplements and guesswork. It takes nuance, expertise, and the right timing. Working with a certified ThaenaBiotic provider keeps your recovery plan safe and strategic.
Whole Essentials Nutrition is a big supporter of “test, not guess.” With the right testing and professional guidance, a precise snapshot of your gut health is possible, and restoration is achievable and sustainable.
How I Help Clients Heal the Gut from the Inside Out
As a holistic nutritionist specializing in functional nutrition gut health, I work with clients who feel dismissed, gaslit, or stuck, A.K.A. people who’ve been told “your labs look fine” while their symptoms continue to impact daily life.
I use a strategic, evidence-based 3-step process to guide healing:
1. Test with the GI-MAP Stool Analysis
Before we jump into treatment, we need to see what’s actually happening inside your gut. The GI-MAP test is a diagnostic tool that gives a full picture of your gut health. It can reveal:
- Infections, overgrowths, and dysbiosis
- Leaky gut and immune markers
- Inflammation and digestive function
- Levels of good vs. harmful bacteria
This is the gold standard for advanced gut testing and is far more revealing than a colonoscopy or general lab work. It’s extremely helpful for identifying the root causes of chronic symptoms and customizing treatment protocols.
2. Treat with Personalized Nutrition and Targeted Supplements
Once we have your GI-MAP results, we design a plan just for you. This may include:
- Whole food nutrition to lower inflammation and rebalance gut flora
- Targeted supplements, like ThaenaBiotic, to support microbiome restoration
- Additional supports like digestive enzymes, binders, or antimicrobial herbs, if needed
This isn’t a trendy protocol. It’s a precise approach backed by data and personalized to your symptoms, sensitivities, and goals.
3. Heal with Long-Term Support
Gut health isn’t a one-and-done project; it’s a process. That’s why my Gut Restore Program provides long-term guidance to help you continue nurturing your gut and feeling your best.
You’ll get:
- Weekly group coaching and check-ins
- Monthly Q&A calls with experts
- Ongoing food and supplement strategy adjustments
As a certified holistic nutritionist and gut health expert in Salt Lake City, I specialize in working with the most sensitive patients. If you’re dealing with chronic symptoms and you’re in Utah, I offer GI MAP testing as a foundational step in my practice. I also work online, so location is not limited!
I’ll be with you every step of the way. I’ll provide the tools, knowledge, and support tailored to your microbiome. This is not your average approach to nutrition. It’s functional nutrition for gut health that puts strategy before supplements.
If you’ve been searching for a ThaenaBiotic provider or want to learn more about how to rebuild your microbiome, you’re in the right place. I’d love to connect to learn more about your gut story, your symptoms, and how we can start restoring your microbiome. Book your discovery call today!
DON’T MISS THIS!
START YOUR PATH TO BETTER HEALTH
Take our free Gut Health Assessment today and discover personalized steps to improve your digestion and well-being. Don’t wait—unlock the key to a healthier you now!